
© Photo: Susan Freundlich
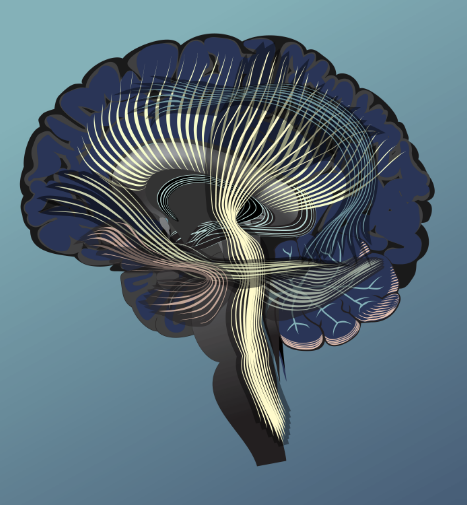
The Traumatic Brain Injury Epidemic
Did you know? Female athletes sustain concussions at higher rates than male athletes.
3.8M
Concussions
in the US each year produced by sports and recreational injuries, according to the CDC.
70M
People
somewhere in the world will experience a TBI each year. Most of these are concussions or mild brain injuries.
38%
Increase
in concussion diagnoses in US emergency rooms from 2007 to 2011. One third were sports related.




One evening, when Seth was biking home, a collision threw him off his bike and into the windshield of an oncoming car. Fortunately, he was wearing a helmet. But the windshield shattered, and blood gushed from his eyebrow. He wanted to continue on his way, but bystanders suggested otherwise.
An ambulance took him to a familiar place, the very medical center where he was in his second year of medical school. They scanned him for injuries, stitched up his face and shoulder, and sent him home.
The next day, he felt worse. For weeks and months, he had headaches, dizziness, episodes of blurry vision, sensitivity to light and sounds, and other difficulties.


© Photo: Susan Freundlich
Reviews of Shaken Brain
A fascinating page turner. Propelled by Dr. Sandel’s exceptional storytelling and clinical expertise, Shaken Brain sheds light on the myths and misunderstandings surrounding concussions, and their consequential impact on so many lives.
![]() Marilyn Spivack, cofounder and past President, Brain Injury Association of America
Marilyn Spivack, cofounder and past President, Brain Injury Association of America
“A thoroughly engaging and enlightening account, this book explores the often perplexing issues and controversies surrounding post-concussion symptoms. A vital read.”
![]() Mel Glenn, MD, Chief, Brain Injury Division, Spaulding Rehabilitation Network
Mel Glenn, MD, Chief, Brain Injury Division, Spaulding Rehabilitation Network
“A valuable resource for patients who have experienced concussion and their families, as well as for the physicians, therapists, and scientists who have made it their life’s work to help them.”
![]() John Leddy, Professor, Medical Director, Concussion Management Clinic, SUNY Buffalo
John Leddy, Professor, Medical Director, Concussion Management Clinic, SUNY Buffalo
Latest Insights
Dr. Sandel maintains an active network with other leading brain injury experts. In this blog, she shares ground-breaking insights and fresh perspectives to help you navigate this complex condition and learn about common concussion symptoms.
Sudden Insights and the Brain: The Aha Moment
The term insight can refer to a variety of human cognitive processes. An insight could derive from logical formations of ideas through analytic reasoning. Another kind of insight, the sudden creative idea, or the unexpected solution to a problem, is referred to as an “aha moment,” or an “aha experience.” Researchers are studying what brain activity underlies insight, and specifically the aha moment, through advanced technologies. This blog provides some possible ways to promote insight and the aha moment in our daily lives and work.
Flying in the Face of Facts: Denialism, Anosognosia, and the Human Brain
When someone refuses to accept an empirically verifiable reality, they call upon irrational thought processes and behaviors that produce denialism. People sometimes process information to reach conclusions driven not by rational analysis, but by specific motivations or beliefs.
The Repercussion Group Issues Urgent White Paper Warning Against “Run It Straight” and RUNIT Championship League
The Repercussion Group, a global coalition of medical and advocacy experts, has issued an urgent White Paper condemning the viral “Run It Straight” challenge and its commercial spin-off, the RUNIT Championship League, as dangerous and unethical. These events, which involve participants colliding at full speed for online entertainment, pose severe risks of brain trauma, spinal injury, and long-term neurodegenerative disease. The group warns that social media platforms are enabling and profiting from this harmful content, often targeting vulnerable individuals. They call for immediate policy action, including bans, content regulation, education initiatives, and research funding, to curb what they describe as a growing public health crisis.
Achieve better health outcomes for patients with brain injuries
Featured info for healthcare professionals