Falls and Brain Injury in Older Adults

If an older adult falls, the risks of a severe injury are more significant than for a young person. Specific symptoms or signs can indicate a severe injury. This might be a fracture, especially if there is underlying osteoporosis. If there was an injury to the head, there might be a brain injury.
Certain “red flags” mean a call to 911. These are a loss of consciousness, confusion, memory problems, agitation, difficulty speaking, dizziness, balance problems, drowsiness, severe headache, vomiting, visual disturbances, or hearing loss.
Symptoms may be delayed for hours or even days after the injury. Certain medications such as anticoagulants (including aspirin) may cause more risk of bleeding in the brain.
Barbara’s Story
In my book, Shaken Brain, I present a story about Barbara, a 72-year-old retired college professor who fell in the bathroom of her home. She had atrial fibrillation and took warfarin, an oral anticoagulant, to prevent a stroke. Barbara moved in with her daughter Diane when she began to develop memory problems. One morning, Barbara tripped and fell, hitting her head on the bathroom sink’s granite counter. Diane heard a noise and rushed into the bathroom. Barbara had a gash on her forehead, but she was conscious and seemed to be thinking and speaking coherently. Diane helped her mother to her feet and nursed her cuts and bruises from the fall.
The following day, things had changed. Diane had to shake her mother to rouse her from sleep. When the paramedics arrived, Barbara was disoriented, and when she got to the hospital, she could no longer speak. Barbara was slipping into a coma.
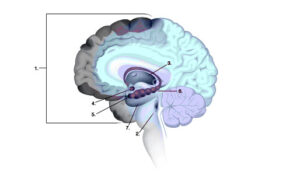
Barbara had experienced a subdural hematoma. This term means that the blood pooled under the dura, the brain’s rigid membrane, because of ruptured blood vessels. It gradually expanded during the night. In older people, subdural hematomas may occur more often than in younger people because the aging brain tends to atrophy and shrink. The blood vessels also shrink and become thinner and tauter—and thus more susceptible to tears.The anticoagulant warfarin also increased Barbara’s risk of having a brain bleed. (See Figure 8 in Shaken Brain)
Subdural Hematomas
A subdural hematoma may form very slowly and diagnosis can be delayed. Symptoms may be mild like those experienced after a concussion. Some people with a small subdural bleed have no symptoms initially, leading caregivers, patients, and even health care providers to believe that the injury is not serious enough to require treatment. Some occur without a blunt head injury or any history of trauma. Sometimes they are found on a CT scan of the brain ordered for other reasons.
Elderly patients have different physiological and psychological needs than younger patients. Some research suggests that even mild TBIs may worsen cognitive decline, including earlier onset of dementia, in the years following the injury. Elderly patients also tend to have several health factors or medications already in play when they fall, complicating the initial injury and ultimately their ability to recover.
Emergency neurosurgery to remove the subdural hematoma saved Barbara’s life. But healing from this injury for an older person remains a longer-term proposition. You can read more about Barbara’s story in my book, Shaken Brain.
Preventing Falls for Older Individuals / Seniors
Falls are the leading cause of traumatic brain injuries (TBIs) in the U.S., and older people like Barbara, especially those with physical or cognitive issues, are most at risk. Falls lead to nearly half of the TBI-related hospitalizations and account for the majority of TBI-related deaths in adults 65 years of age and older. Many older adults have patterns of frequently falling, too. What makes older people more likely to fall, and how can these falls be prevented?
Falls in older individuals are often caused by more than one factor. Older individuals have age-related changes such as vision, hearing, and cognitive impairments. They may have reduced sensation in their feet, poor postural control and balance problems, generalized weakness, and other neurologic or muscle and joint problems that can put them at risk of falling. Medications that cause issues with awareness, balance, or reaction-time can contribute to a risk of falling. Environmental factors such as an uneven floor, rug, or pavement surface can also contribute to risks. Situational factors such as moving too quickly or not turning lights on when entering a room might be part of a risk equation. Living alone and a diagnosis of depression were associated with higher fall risk in some studies. If there is a suggestion that the older person lost consciousness and then fell, perhaps from a drop in blood pressure or other cause, a further workup for a cause or causes is imperative.
Here are some specific factors that may contribute to falls in older people that are amenable to interventions:
Mobility problems(related to gait, balance, strength, flexibility, endurance, pain):
Physicians must carefully examine motor and sensory function and joints, especially in the legs and feet, and provide treatments. Physical and occupational therapists and podiatrists can help to evaluate and recommend preventive strategies. Sturdy, anti-slip footwear and mobility aids such as canes or walkers might be essential interventions.
Medication review
Physicians should determine if all medications are necessary and discontinue those not needed. Reducing doses of required medications that may contribute to risk can be critical, too. Patients on platelet aggregation inhibitors and oral anticoagulants should be closely monitored.
Bladder and bowel function and nutrition assessment
Bedtime diuretics should be discontinued if possible. Low blood pressure or orthostatic hypotension (a drop in blood pressure when standing up) can contribute to falls. Inadequate nutrition or dehydration may contribute to low blood pressure.
Vision and hearing evaluations
Are eyeglass prescriptions up-to-date? Are progressive lenses causing problems? Would cataract surgery help? Would a hearing aid help to increase awareness of surroundings and prevent injuries?
Diagnosis of mood disorders
Depression is a risk factor for falls. Physicians should screen for depression and refer for treatment.
Environmental assessment
A home assessment should include the evaluation of furnishings and flooring, especially rugs. Removal of throw rubs and the addition of grab bars in the bathroom may be very beneficial. Alert systems and motion detectors for lighting systems can be preventive, too.
There is more information about preventing falls in older people on the CDC and Academy of Physical Medicine and Rehabilitation (AAPM&R) websites:
You Might Also Like
Self-Reported Concussion Symptoms are Key to Evaluation & Diagnosis
To properly diagnose a concussion and devise a treatment plan requires a thorough physician evaluation, a symptom checklist or an interview, or both, followed by a comprehensive cognitive and physical examination. Download a pocket guide that helps patients prepare for being evaluated.
Mood Disorders Such as Depression Can Complicate a Brain Injury
A traumatic brain injury can be associated with depression or another mood disorder, possibly because of the disruption of brain chemicals.
Repetitive Brain Trauma and Chronic Traumatic Encephalopathy (CTE)
There’s a link between chronic traumatic encephalopathy (CTE) and repetitive brain injuries that occur in boxing and American football. This is a progressive neurodegenerative disorder that can lead to severely-disabling neurologic and psychiatric disorders. Learn about the science, diagnostic criteria for traumatic encephalopathy syndrome (TES), and possible treatment approaches.
Coma and Other Disorders of Consciousness
What happens to the brain after a severe brain injury that renders a person unconscious or “comatose”? Learn the meaning of other terms that describe patients who have disorders of consciousness: the minimally conscious state, cognitive-motor dissociation, covert consciousness, and unresponsive wakefulness syndrome (vegetative state). Researchers are studying advanced technologies evaluating patients with disorders of consciousness, and there are new U.S. and European guidelines that are helping to standardize care and advance the field of brain injury.
Keep up to date
Get updates on the latest in concussion, brain health, and science-related tools from Dr. Elizabeth Sandel, M.D.
By clicking SIGN UP, you agree to receive emails from Dr. Sandel and agree to our terms of use and privacy policy.
Get the book!