Why is “Post-Concussion Syndrome” Controversial?

We do not yet have a clear understanding of what happens in the brain immediately after a concussion and over the days and months that follow, especially for those patients whose symptoms persist. Post-concussion symptom rates vary greatly among research studies, likely because the populations studied are diverse and so are the diagnostic criteria and timing of assessments. The wide variation in symptom rates highlights the fact that there is a lot we still don’t know about concussions.
Even the terminology has not been settled: we continue to refer to “post-concussion syndrome” (PCS) or “post-concussion disorder” or, variously, postconcussional syndrome or disorder. Clinicians and researchers have debated these terms since they were first used decades ago. I mentioned the controversies in a previous blog. Here I delve deeper into the issue.
Here are some explanations for the controversies:
PCS Symptoms Are Nonspecific
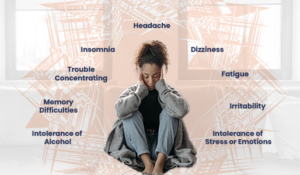
Some of the most common symptoms described by people in the days after a concussion include:
- Headaches
- Neck pain
- Dizziness
- Poor memory
- Poor concentration
- Fatigue
- Sleep problems
- Irritability
- Anxiety
- Sensitivity to light
- Sensitivity to noise
- Visual disturbances
These are nonspecific symptoms, however, meaning they can be caused by any number of underlying problems, and some may become chronic. As a result, there are people who may fit the criteria for a concussion-related disorder despite having had no history of a concussion. Some clinicians question whether it’s clinically helpful to define a condition so broadly that it can apply to people who are clearly not candidates for it.
The Risk of PCS Misdiagnosis Is Substantial
Because these symptoms are nonspecific and overlap with symptoms of many other conditions, it’s difficult for physicians to definitively diagnose the condition that has been called PCS.
In addition, patients who have sustained a mild TBI may be diagnosed with concussion-related symptoms when they are actually suffering from post-traumatic stress disorder (PTSD), depression, anxiety, or a condition with a strong component of chronic pain such as chronic fatigue syndrome or fibromyalgia. Conversely, patients may be diagnosed with one of those conditions when they are actually experiencing the effects of a brain injury. Or a patient may suffer from more than one condition, such as depression, that exacerbates the symptoms that emerge after a concussion.
PCS is Not Really a “Syndrome”
In medical terms, a “syndrome” is a set of symptoms that occur together and are all related to the same underlying cause. The appearance of one symptom in a syndrome means it’s highly likely that the other symptoms will appear, too.
But in the case of concussions, the lists of symptoms and their possible combinations is so large that there’s controversy over whether “syndrome” is the correct label for it. Symptom clusters often differ among people who have had concussions. For example, some may have more physical (somatic) symptoms such as headaches and dizziness, while others may experience more emotional symptoms such as irritability or anxiety. Another group may have cognitive symptoms such as difficulty concentrating or remembering information. And many individuals experience combinations of somatic, emotional, and/or cognitive symptoms.
This is why some clinicians began to use the term “disorder,” a more general term.
Is PCS Physiological or Psychological?
Adding to the difficulties is the fact that there may not be a clear etiology for post-concussion symptoms – that is, we don’t know the exact physiological mechanisms in the brain that cause, for example, post-traumatic headaches or sleep disturbances.
Researchers have uncovered evidence that psychological factors heavily influence the development of a chronic condition following a concussion. Clinicians must always consider pre-existing psychological issues and post-concussion stressors when they diagnose a patient diagnosis and develop a treatment program.
No Universally Accepted Criteria for PCS Diagnosis
Clinicians disagree on the criteria for a diagnosis of a post-concussion disorder. In fact, the two widely referenced works used by physicians and other healthcare providers, the International Classification of Diseases (ICD) and the Diagnostic and Statistical Manual (DSM) vary in their criteria for diagnosis, and their definitions have changed over time.
The term “postconcussional disorder” was listed in the DSM-IV but is absent from the current edition – the DSM-V. Instead, the new edition categorizes symptoms that persist after the initial trauma as “mild neurocognitive disorder which may be caused by intracranial injury.” Unfortunately, this newer DSM edition bases its definition for all the people who have chronic, persistent symptoms after a concussion solely on evidence of cognitive dysfunction, when such a decline may not occur, or may not be the primary symptom.
Changes to the ICD definition have also evolved over time. In the late 1990s up to the ICD-10 edition, the definition of “postconcussional disorder” or “postconcussional syndrome” was criteria-based. Three of these eight symptoms had to be present for more than a month after a concussion: headaches, dizziness, fatigue, irritability, difficulty in concentration and performing mental tasks, impairment of memory, insomnia, and reduced tolerance to stress, emotional excitement, or alcohol.
Then the latest edition of the ICD, the ICD-11, altered its definition to match that of the DSM-V. Neither reference work now uses the terms postconcussion syndrome or postconcussional disorder.
Treating Post-Concussion Symptoms
Despite how textbooks and coding manuals describe their symptoms, or how various medical professionals view these controversies, the fact is that many people suffer from an array of symptoms after their initial concussion. Despite the controversies, there continue to be physicians and other clinicians devoted to the medical treatment and rehabilitation of people with persistent symptoms.
A biopsychosocial approach to treating a patient’s symptoms with the availability of a multi-disciplinary team to treat patients works best given this stage of our knowledge. We await basic scientific and medical advances that can lead to the sort of disease-modifying treatments available for many other medical conditions so that we can do more than just treat symptoms.
You can learn more about the evaluation and treatment of post-concussion symptoms by watching my interviews with clinicians (below).
You Might Also Like
Discussion with Dr. Ernie Bryant
Dr. Ernie Bryant is a neuropsychologist with decades of experience treating people with brain injuries of all severities, including concussion. What is a neuropsychological evaluation? Dr. Bryant presents a case of a worker whose neuropsychological examination was complex as is often the case with brain injuries, especially concussions.
Treatment and Prognosis after a Concussion
Learn about treatments for post-concussion symptoms—including medication, various rehabilitation therapies, neuropsychology, and potentially some complementary therapies—as well as factors related to longer concussion recovery times.
What is Post-Concussion Syndrome?
I recently talked with journalist Nathaniel Parish Flannery who writes about cycling. He was writing an article about pro cyclist Ian Boswell. Boswell had a crash in 2019 that resulted in long-term concussion symptoms. Flannery found our conversation and my book, Shaken Brain, very helpful, and he tells Boswell’s story in…
Keep up to date
Get updates on the latest in concussion, brain health, and science-related tools from Dr. Elizabeth Sandel, M.D.
By clicking SIGN UP, you agree to receive emails from Dr. Sandel and agree to our terms of use and privacy policy.
Get the book!