How Does Brain Trauma Affect Brain Hormones?
The Role of the Pituitary Gland & Hypothalamus
The pituitary gland regulates many essential hormones for our existence as well as our health and well-being. The tiny gland sits in the sella turcica, a structure within the sphenoid bone, a bone that connects the facial bones to the skull bones. The pituitary gland is closely connected with another part of the brain – the hypothalamus. These two structures are vulnerable to head and face trauma and a lack of blood supply, such as during a cardiac arrest. Blast injuries from explosive devices can also damage the pituitary and related structures.
The hypothalamus releases hormones (called releasing hormones) that act on the pituitary gland. The pituitary gland, in turn, acts on other organs in the body. See Figure 1.
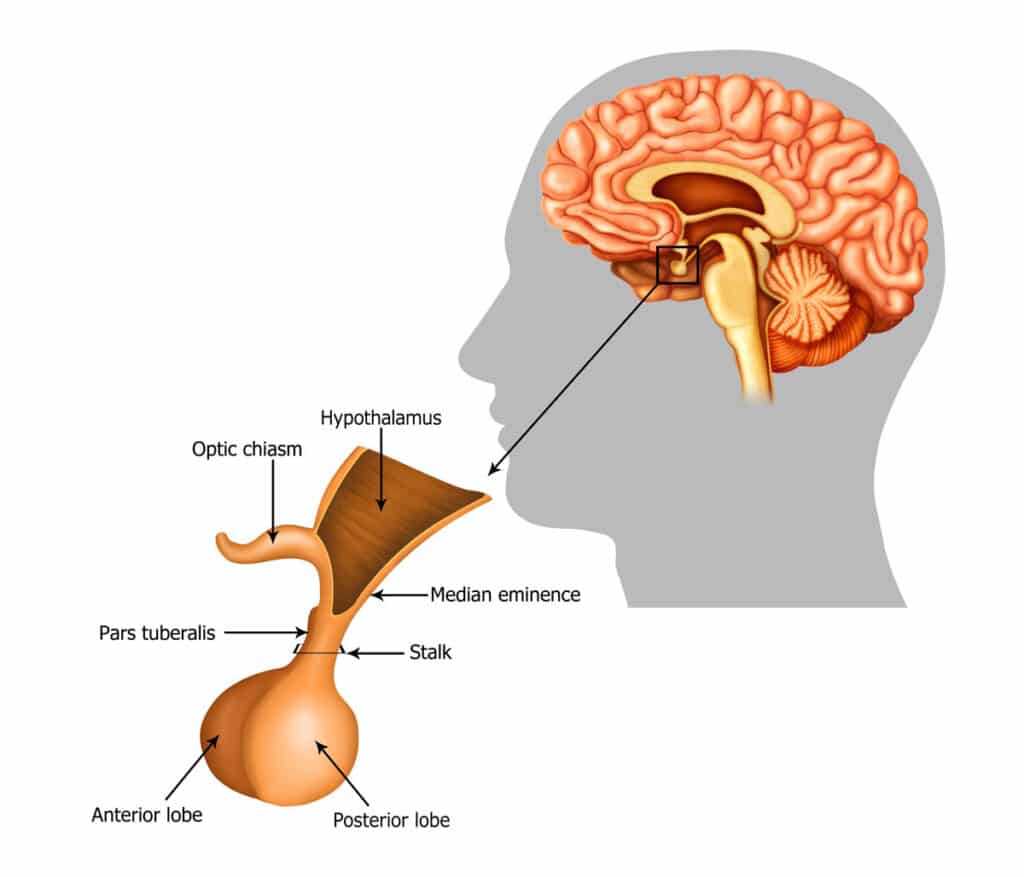
The Posterior and Anterior Pituitary
There are two parts of the pituitary with very different anatomic and functional characteristics.
The posterior pituitary (the part closer to the back of the head) secretes two stimulating hormones: antidiuretic hormone (ADH), which acts on the kidneys to regulate salt and water content in the body, and oxytocin which stimulates the uterus to contract during labor and childbirth, and breast tissue to stimulate milk production after childbirth.
The anterior pituitary (the part of the gland closer to the face) secretes stimulating hormones that act on various bodily structures to stimulate the production of other hormones. For example, thyroid-stimulating hormone (TSH) acts on the thyroid gland to stimulate thyroid hormone production. There are feedback loops that tightly regulate these systems to keep the levels of hormones in the normal ranges.
Hormones & Brain Injury: Controversies and Challenges
Evaluating and treating people with hormonal deficiencies after traumatic brain injury (TBI) can be very challenging. Over the decades, research designs have varied in terms of the age of subjects, the injury severity, and the time points of evaluation and testing protocols. The prevalence of pituitary abnormalities after TBI varies greatly across research studies, from a mere 1% to three-quarters of TBI patients being reported as potentially affected!
Some acute deficiencies may resolve, but other deficiencies may emerge in the chronic stages after brain trauma. A recent research study (with a meta-analysis of other research studies) led the authors to conclude that approximately one-third of TBI patients have persistent anterior pituitary dysfunction 12 months or more following the injury.
Acute Hormonal Abnormalities Can Be Life-Threatening
Panhypopituitarism (deficiency in all hormones produced by the pituitary) can occur after severe TBIs and is life-threatening. It is a condition that must be considered in any trauma patient with low blood pressure, low salt and glucose in the blood, and low body temperature.
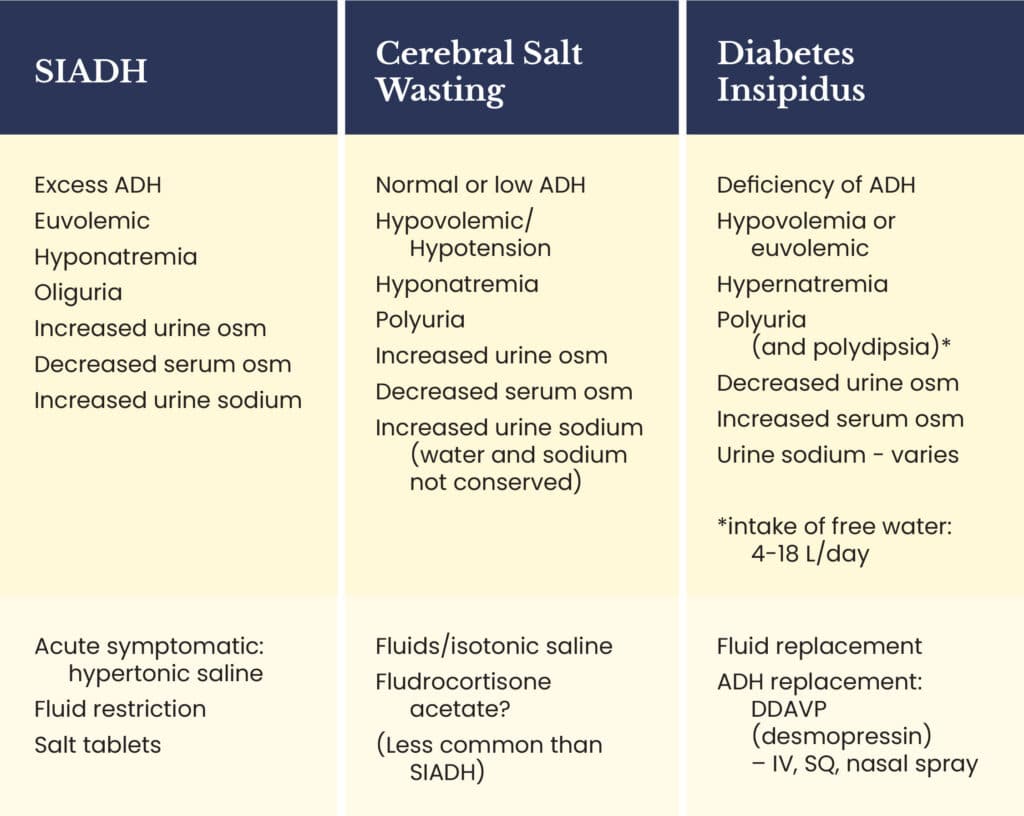
In the acute stages after a TBI, abnormalities in the posterior pituitary result in too much or too little anti-diuretic hormone (ADH). Diabetes insipidus (DI) is a condition resulting from a deficiency of ADH and is a life-threatening condition because of the severe loss of water from the body. The syndrome of inappropriate secretion of ADH (SIADH) and cerebral salt wasting syndrome are more common and require laboratory evaluation and prompt treatment because of the imbalance of water and salt in the body. See Table 1 for the differences in these three posterior-pituitary conditions.
Evaluation and Treatment of Anterior Pituitary Deficiencies
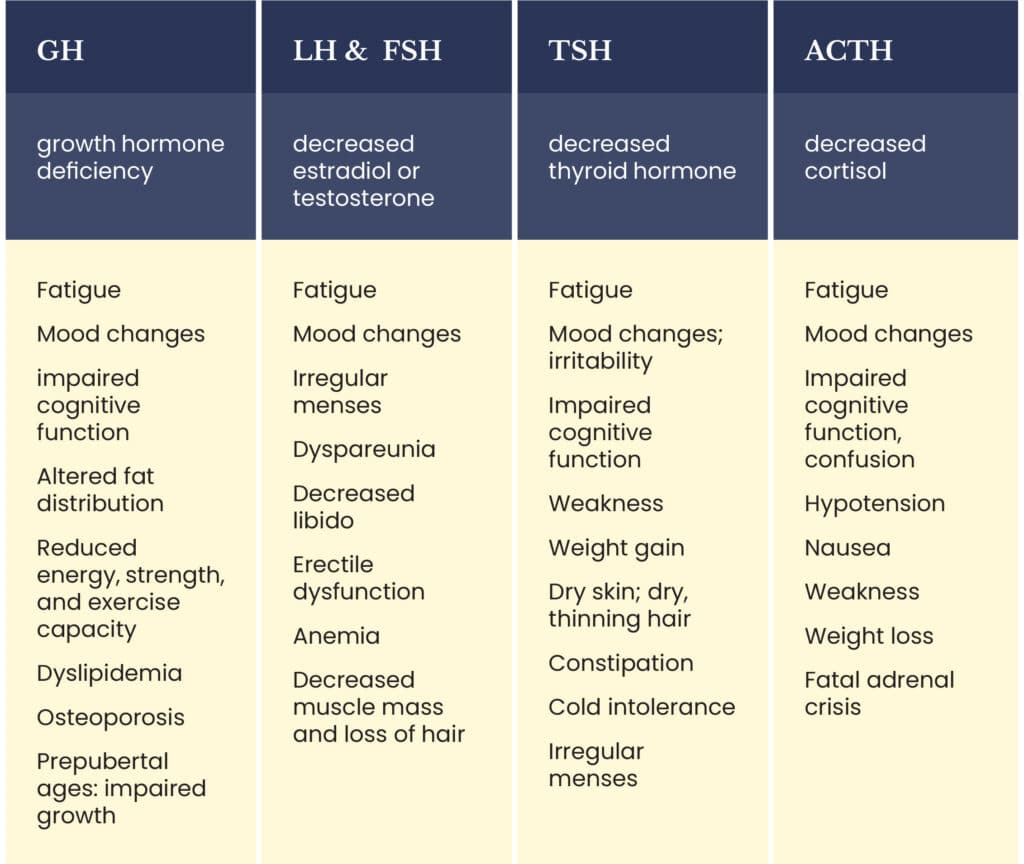
Many of the subtle symptoms or signs of an anterior pituitary deficiency such as fatigue or cognitive problems are not always due to a hormonal abnormality. See Table 2 for a list of the symptoms and signs that might mean there is a hormonal system abnormality.
Unfortunately, neuroendocrine clinical practice guidelines for screening patients after a TBI have been inconsistent over many years. New York University Endocrinologist, Dr. Tamara Wexler, specializes in treating patients with TBI and hormonal abnormalities. In a textbook chapter in Brain Injury Medicine, third edition, she recommends screening TBI patients for ACTH and TSH deficiencies in the acute period, treating the deficiencies if present, and then reassessing at 6 and 12 months. She also recommends screening at 3, 6, and 12 months for chronic hormonal deficiencies and treating if a patient is symptomatic. These hormonal evaluations are complicated and require an endocrinologist to design and implement the best protocols for individual patients.
For patients with more than one hormonal deficiency, a stepwise protocol for treatment is critical. For patients with adrenal insufficiency, cortisol must be replaced first with prednisone or hydrocortisone. Thyroid hormone is replaced next with levothyroxine once adrenal insufficiency is treated. Abnormalities of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) and the corresponding deficiencies of estradiol or testosterone are addressed differently in men and women and with a different regimen if fertility is desired. Growth hormone is replaced last after adrenal, thyroid, and gonadal system abnormalities are addressed.
For children with TBI, hormone deficiencies can affect growth and maturation, and pediatric endocrinologists can determine the best screening and treatment protocols.
Concussion & Hormones
Dr. Wexler addressed this important topic in an interview with Julian Szieff, a Concussion Alliance Intern. See the interview here.
You Might Also Like
Mood Disorders Such as Depression Can Complicate a Brain Injury
A traumatic brain injury can be associated with depression or another mood disorder, possibly because of the disruption of brain chemicals.
A Neuropsychologist is a Brain Injury Expert
Neuropsychologists are psychologists with training in brain functioning. They offer evaluations, education, and counseling for people with brain injuries. Health can educators help, too, because education is a key part of concussion care.
Keep up to date
Get updates on the latest in concussion, brain health, and science-related tools from Dr. Elizabeth Sandel, M.D.
By clicking SIGN UP, you agree to receive emails from Dr. Sandel and agree to our terms of use and privacy policy.
Get the book!