Archive
Brain Injury Diagnosis & Treatment
How are traumatic brain injuries diagnosed, and what treatment is recommended for concussions and other brain injuries?
AMA Hub offers Concussion CME
The AMA Ed Hub has posted the CME program produced by Dr. Sandel and Concussion Alliance.
Is There a Connection Between Mild TBI and Mental Health Disorders in Adults and Children?
In a recent study, researchers at Kaiser Permanente found that risks for affective and behavioral disorders were significantly higher in the years post-injury for children and adolescents with a history of mTBI—especially for 10- to 13-year-olds. They emphasize the importance of regular interval screening for affective and behavioral disorders in children and adolescents who sustain a mild TBI. This post includes a slide presentation and Q & A with two of the researchers, Richard Delmonico, PhD, and Brian Theodore, PhD.
Concussion Alliance Co-Founders Interviewed for Slate Article
More and more journalists are writing about concussion, in many cases because they have had a concussion themselves or have friends or relatives who have experienced one. In March, 2024, Isobel Whitcomb interviewed Concussion Alliance co-founders Conor Gormally and Malayka Gormally for an article in Slate. It is concerning that bad medical advice (“just rest”) is still being given to concussion patients as is clear in Whitcomb’s story.
Concussion Care Highlighted in The Atlantic and Bloomberg News
I collaborated recently with Conor Gormally of Concussion Alliance to advocate for individualized and comprehensive concussion care in mainstream news stories with journalists who recounted personal stories of concussion. Here’s what The Atlantic and Bloomberg published.
The 6th International Consensus Statement on Concussion in Sport–What’s New?
The Statement summarizes scientific research and provides some updated recommendations for athletes at risk for concussions. But, it’s been mired in controversy regarding the strict criteria governing which research was included. Read Dr. Sandel’s insights into the process and conclusions.
What Is Cognitive Rehabilitation Therapy?
Cognitive Rehabilitation Therapy (CRT) is an evidence-based approach to addressing multiple cognitive impairments caused by a traumatic brain injury. Restorative CRT strengthens cognitive abilities, and compensatory CRT provides strategies to reduce the impact of deficits.
Patient-Centered Concussion Care
Presenting to the physical medicine and rehabilitation (PM&R) residents at the UC Davis School of Medicine sparked a lively exchange about patient-centered concussion care. Learn more about the challenges and possibilities for transforming concussion care.
Evaluating and Treating Headaches After Brain Injury
Headaches are extremely common after a traumatic brain injury, but there are various treatments that vary depending on the phenotype or cause.
Post-Traumatic Headaches: Not Just One Type or Treatment
Headaches must be evaluated with a comprehensive history and physical examination. There are many options for treatment, but diagnosis has to be the first step.
Check the Neck after a Brain Injury
Whiplash and cervical strain occurs when a person’s head and neck are forced back and forth, injuring soft tissues of the neck. They are common after brain injuries.
Three Alternative Treatment Modalities to Ease Brain Injury Associated Symptoms
Conventional treatments like medications may not help symptoms after a brain injury. Complementary or alternative treatments may help.
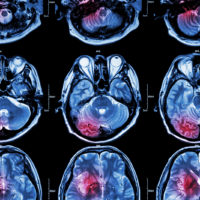
Brain Imaging after an Injury
CT and MRI scans are the most common imaging modalities to evaluate people with traumatic brain injury, but advanced imaging methods are more promising for diagnosis and prognosis. However, interpretations of findings can vary.
Keep up to date
Get updates on the latest in concussion, brain health, and science-related tools from Dr. Elizabeth Sandel, M.D.
By clicking SIGN UP, you agree to receive emails from Dr. Sandel and agree to our terms of use and privacy policy.